乾眼症 (DED) 是一種高度流行的眼部疾病,其特徵是淚膜和眼表穩態的改變。根據香港中文大學 2022 年的一項調查,約有 30% 的人口患有乾眼症。值得注意的是,80% 的乾眼症病例是脂質缺乏性或蒸發過強型乾眼症,是由瞼板腺功能障礙 (MGD) 引起的。因此,瞼板腺功能障礙影響著數百萬人,尤其是在亞洲國家。
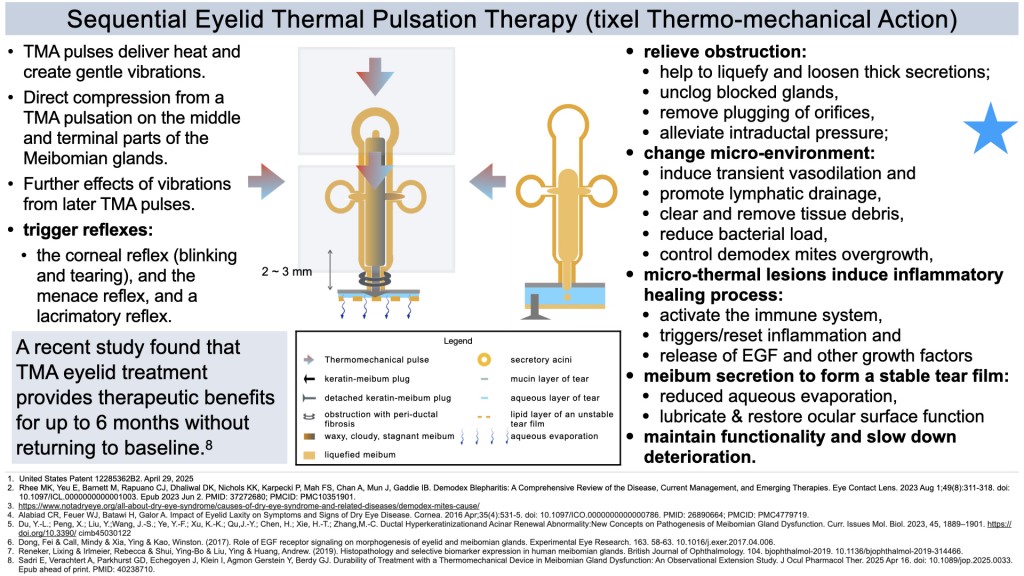
瞼板腺功能障礙 (MGD) 患者的眼瞼油脂分泌腺無法分泌足夠或適當的油脂,從而導致乾眼症狀。這些位於眼瞼邊緣的腺體負責分泌瞼脂,這種油性物質可以保護淚膜,防止淚膜過快蒸發,並保持眼部濕潤健康。
瞼板腺功能障礙 (MGD) 可發生在所有年齡層的人群中,尤其是 60 歲以上的人。導致 MGD 的因素有很多,包括老化、荷爾蒙變化、低濕度以及低 Omega-3 脂肪酸或高 Omega-6 脂肪酸的飲食。
其他促成因素包括配戴隱形眼鏡以及某些局部或全身用藥。長時間使用電子設備會導致眨眼頻率降低和眼瞼閉合不全,進而導致淚膜蒸發增加、不穩定,以及淚液滲透壓升高。長時間使用螢幕也可能是兒童和青少年乾眼症 (DED) 發病率上升的一個因素。
在瞼板腺功能障礙 (MGD) 病例中,由眼瞼中的瞼板腺分泌的油性分泌物(稱為瞼脂)分泌份量不足且成分改變。這會導致分泌物增厚、混濁且停滯,更難以擠出。如果沒有足夠的油脂分泌,由黏蛋白、水和油脂組成的健康淚膜層就無法正常形成。
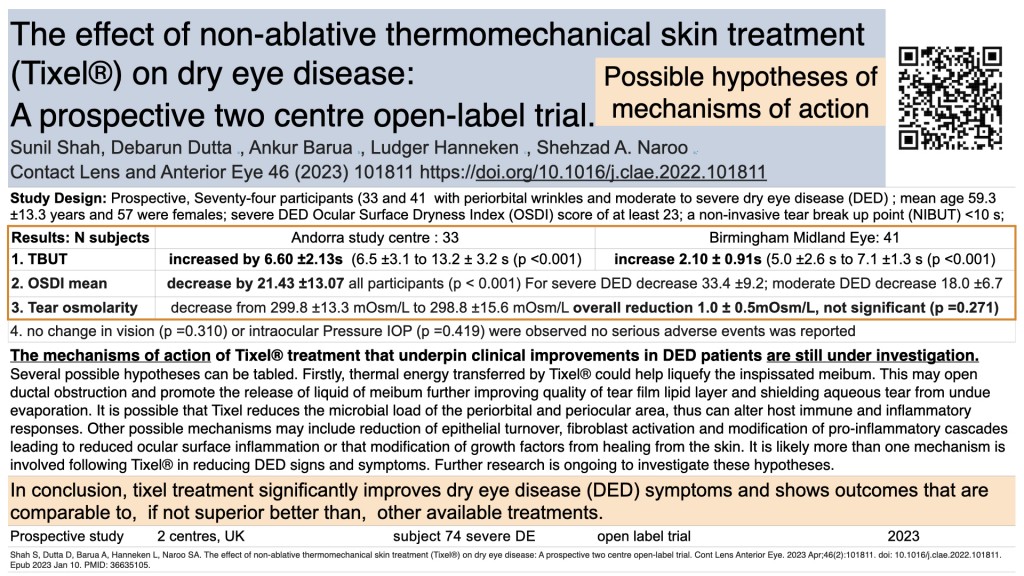
促成因素包括淚膜不穩定、水份蒸發率增加、乾燥、淚液高滲透壓、發炎。眼球表面潤滑不足,導致眼瞼和眼球之間產生摩擦,令眼表細胞受損。這些問題會導致淚液代償性分泌過剩,從而形成乾眼症 (DED) 的持續循環。
乾眼症 (DED) 的眼睛症狀包括乾澀、眼部異物感、眼部疲勞、眼紅、灼熱或疼痛、視力模糊、畏光以及作為代償反應的過度流淚。 DED 也與眼瞼發炎和感染(例如瞼緣炎)以及蠕形蟎蟲感染有關。
總結: 瞼板腺功能障礙 (MGD) 是一種慢性進行性疾病,會危害眼表健康。如果不及時治療,MGD 可能會惡化,導致嚴重症狀、持續不適、角膜損傷、眼部感染以及潛在的嚴重視力障礙。優先考慮有效的醫學治療對於確保您的眼部健康和維持生活品質至關重要。
Dry eye disease (DED) is a highly prevalent ocular condition that is characterised by alterations in the homeostasis of the tear film and the ocular surface. According to a 2022 survey conducted by the Chinese University of Hong Kong, approximately 30% of the population suffers from DED. Notably, 80% of DED cases are lipid-deficient or evaporative dry eye, which is caused by Meibomian gland dysfunction (MGD). As a result, meibomian gland dysfunction affects millions of people, especially in Asian countries.
In patients with Meibomian gland dysfunction (MGD), the oil-secreting glands in the eyelids fail to produce enough oil or produce the wrong type of oil, resulting in dry eye symptoms. These glands, located at the edges of the eyelids, are responsible for creating meibum, an oily substance that protects the tear film. This helps prevent the tear film from evaporating too quickly, keeping the eyes moist and healthy.
Meibomian Gland Dysfunction (MGD) can occur in individuals of all age groups, especially in those over 60. Several factors contribute to MGD, including aging, hormonal changes, low humidity, and diets that are low in omega-3 fatty acids or high in omega-6 fatty acids.
Other contributing factors include the use of contact lenses and certain topical or systemic medications. Extended use of electronic devices can lead to decreased blink rates and incomplete eyelid closure, which results in increased evaporation and instability of the tear film, as well as higher tear osmolarity. Prolonged screen time may also be a factor in the rising rates of dry eye disease (DED) among children and young adults.
In cases of Meibomian Gland Dysfunction (MGD), the oily secretion known as meibum, which is produced by the meibomian glands in the eyelids, is often insufficient in quantity and altered in composition. This leads to a thickened, cloudy, and stagnant secretion that is more difficult to express. Without adequate oil, the healthy layers of the tear film—comprising mucin, water, and oil—cannot form properly.
Contributing factors include tear film instability, increased evaporation rate, dryness, tear hyperosmolarity, and inflammation. Inadequate lubrication of the eye surface causes friction between the eyelid and eyeball, which damages the cells on the eye surface. These problems lead to compensatory overproduction of tears, which creates a perpetuating cycle of dry eye disease (DED).
Ocular symptoms of Dry Eye Disease (DED) can include dryness, a gritty sensation, eye fatigue, redness, burning or pain, blurred vision, sensitivity to light, and excessive tearing as a compensatory response. DED is also associated with eyelid inflammation and infections, such as blepharitis, as well as infestations by Demodex mites.
Summary: Meibomian gland dysfunction (MGD) is a chronic, progressive disease that compromises the health of the ocular surface. If left untreated, MGD can worsen, leading to severe symptoms, ongoing discomfort, corneal damage, eye infection, and potentially serious visual impairment. Prioritizing effective medical treatment is critical to ensuring your eye health and maintaining quality of life.