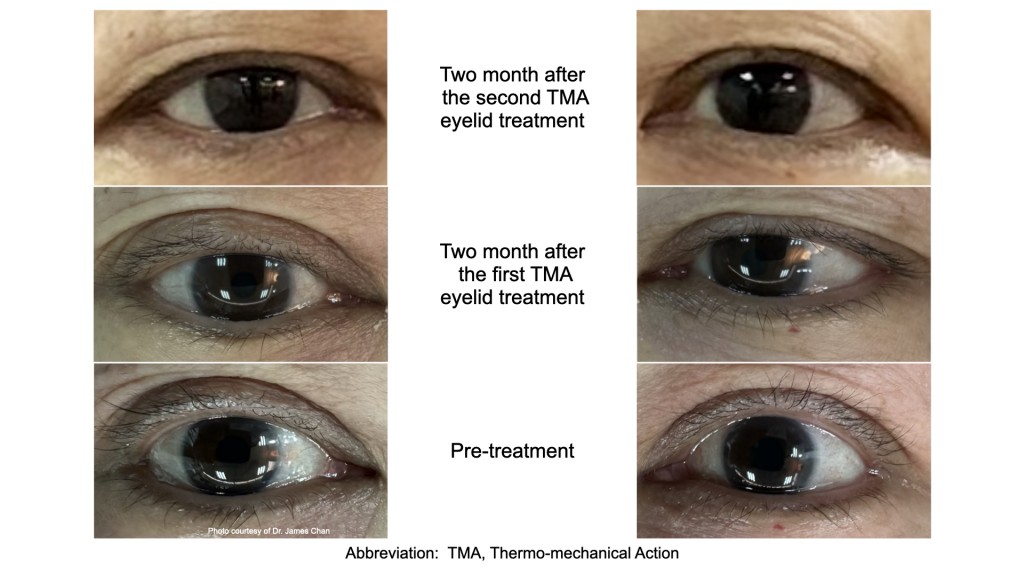
This is a set of clinical photos of Thermomechanical Action (TMA) technology, an effective treatment for evaporative dry eye disease, Demodex blepharitis, and meibomian gland dysfunction (MGD). MGD is the commonest cause of dry eye disease. MGD is a common cause of blepharitis and is often associated with Demodex infestation.
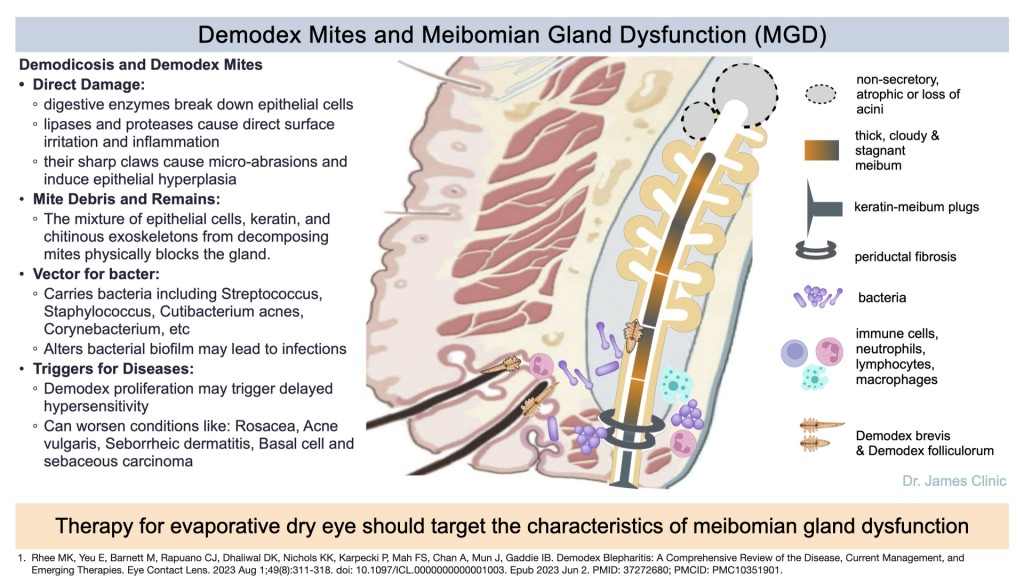
In humans, there are two types of demodex mites on the skin, Demodex folliculorum and Demodex brevis. Demodex folliculorum mites are longer and primarily cluster in human hair follicles, particularly on the face and eyelids, inhabiting the eyelash follicles. They are also found in the sebaceous glands and Meibomian glands. Demodex brevis mites are shorter and exist solitary in the meibomian glands of the eyelids. These mites are believed to contribute to meibomian gland dysfunction (MGD), which can cause dry eye symptoms. Demodex brevis infests the meibomian glands, which produce oil (sebum) that lubricates the eye and helps keep the tear film stable.
Demodex mites are common commensals, meaning they can be present on the skin without causing any symptoms. However, the overgrowth of Demodex mites causes problems like blepharitis, dry eyes due to meibomian gland dysfunction, and rosacea. Demodex blepharitis is especially common in patients over the age of 60.
The following photo is the eyelid of a 65-year-old lady suffering from dry eye disease with compensatory watery tearing. There is evidence of a Demodex mite infestation. These tiny, microscopic parasites live in or near hair follicles, particularly around eyelashes and eyebrows. Cuffing, seen here, is a classic symptom of Demodex overpopulation. The accumulation of degenerated, hyperkeratinized cellular debris with sebum and lipid creates the familiar sign of cuffs, cylindrical dandruff, or “sleeves” commonly seen at the base of the lashes in patients who have D. folliculorum infestation. There is also some debris on the ocular surface, which signifies an unhealthy status of the ocular surface.
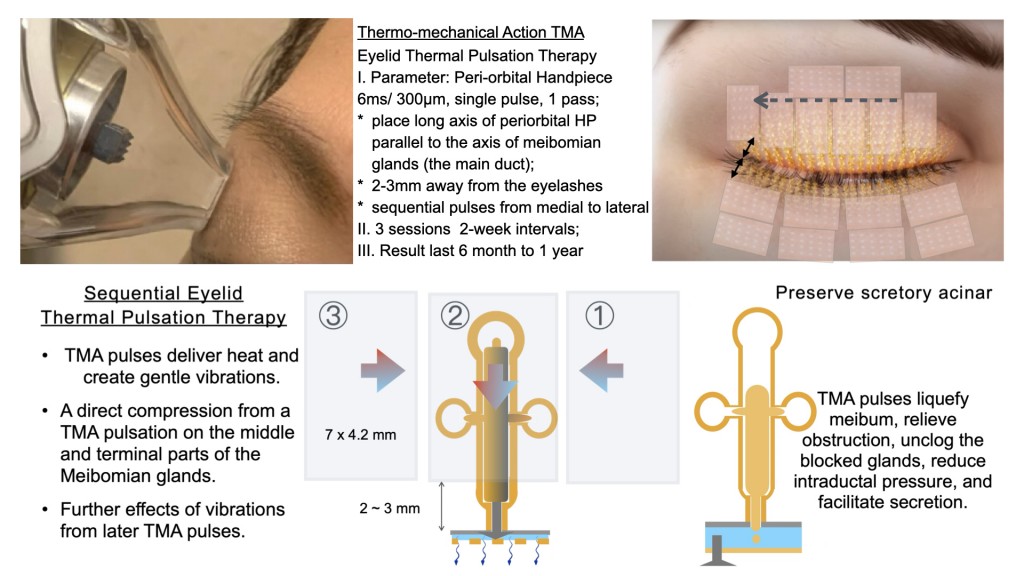
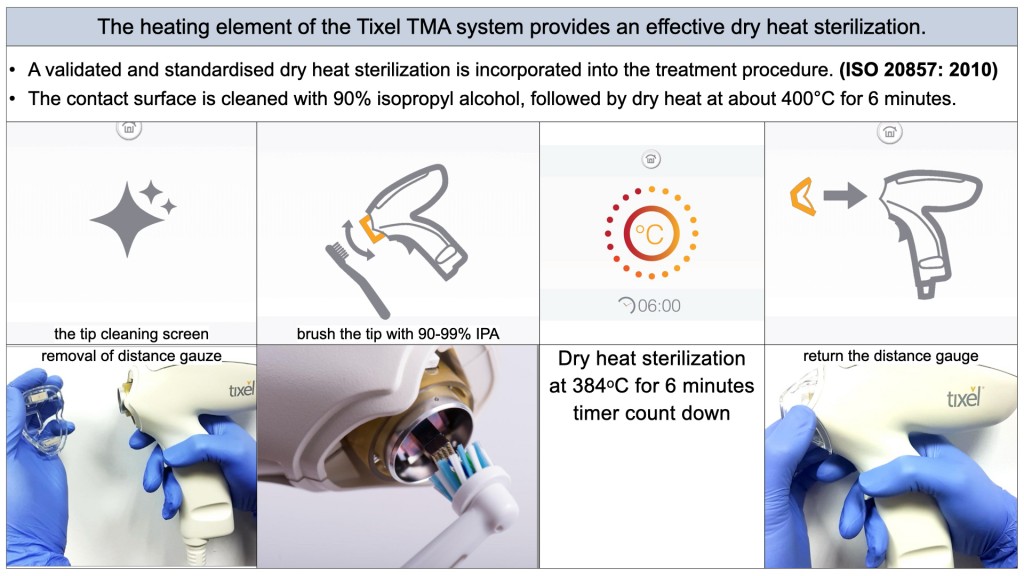
The patient had one session of tixel treatment with the Thermo-mechanical Action (TMA) of the eyelid, a USA FDA-cleared indication. Following the treatment, her dry eye symptoms and inflammation from blepharitis progressively improved. Two months after the procedure, the number of Demodex mites on her eyelid significantly decreased. The dry eye symptoms were alleviated. As a result, the patient no longer required eyedrops for her dry eye condition post-treatment.
A recent clinical study * found that the thermomechanical device TMA is safe and effective for improving signs and symptoms of evaporative dry eye disease in MGD, with benefits lasting up to 6 months. No ocular adverse effects were reported.

Post-treatment photo. Tixel Eyelid Thermal Pulsation Therapy with the Thermo-mechanical Action (TMA) dry eye disease Relief. Two months after the procedure, the eyelid is healthy without overgrowth of demodex mites.
這是熱機械作用 (TMA) 技術的一組臨床照片證據,該技術可以有效治療蒸發過強的乾眼症、蠕形蟎性瞼緣炎和瞼板腺功能障礙。瞼板腺功能障礙是乾眼症最常見的原因, 也是瞼緣炎的常見原因,通常與蠕形蟎蟲感染有關。
在人類中,皮膚上有兩種類型的蠕形蟎,毛囊蠕形蟎和短蠕形蟎。毛囊蠕形蟎較長,主要聚集在人類的毛囊中,尤其是臉部和眼瞼,棲息於睫毛毛囊。它們也存在於皮脂腺和瞼板腺中。短蠕形蟎體型較短,單獨存在於眼瞼的瞼板腺。這些蟎蟲被認為會導致瞼板腺功能障礙(MGD),進而引起乾眼症症狀。短蠕形蟎寄生於瞼板腺,瞼板腺會產生油脂(皮脂),潤滑眼睛並幫助維持淚膜穩定。
蠕形蟎是常見的共生體,這意味著它們可以存在於皮膚上但不會引起任何症狀。然而,蠕形蟎的過度生長會引起瞼緣炎、瞼板腺功能障礙引起的眼睛乾澀以及酒渣鼻等問題。蠕形蟎性瞼緣炎在 60 歲以上的患者中尤其常見。
下圖是一位65歲患有乾眼症的女士的眼瞼,並伴隨著代償性流淚。有證據顯示有蠕形蟎感染。這些微小的寄生蟲生活在毛囊內或附近,尤其是睫毛和眉毛周圍。這裡看到的袖口是蠕形蟎過度繁殖的典型症狀。退化的、角質化的細胞碎片與皮脂和脂質一起積聚,形成了我們熟悉的袖口、圓柱形頭皮屑或「袖子」症狀,常見於感染毛囊蠕形蟎的患者的睫毛根部。眼表上還存在一些碎屑,顯示眼表狀態不健康。
該患者接受了一次眼瞼熱機械作用 (TMA) 的 tixel 治療,這是美國 FDA 批准的適應症。經過治療,她的乾眼症症狀和瞼緣炎引起的發炎逐漸改善。手術兩個月後,她眼瞼上的蠕形蟎蟲數量明顯減少。乾眼症狀得到緩解。結果,治療後患者不再需要滴眼藥水來治療乾眼症。
最近的臨床研究發現,TMA 熱機械眼瞼治療可安全有效地改善 MGD 蒸發性乾眼症的徵兆和症狀,且療效可持續長達 6 個月。報告沒有發現眼部不良反應。
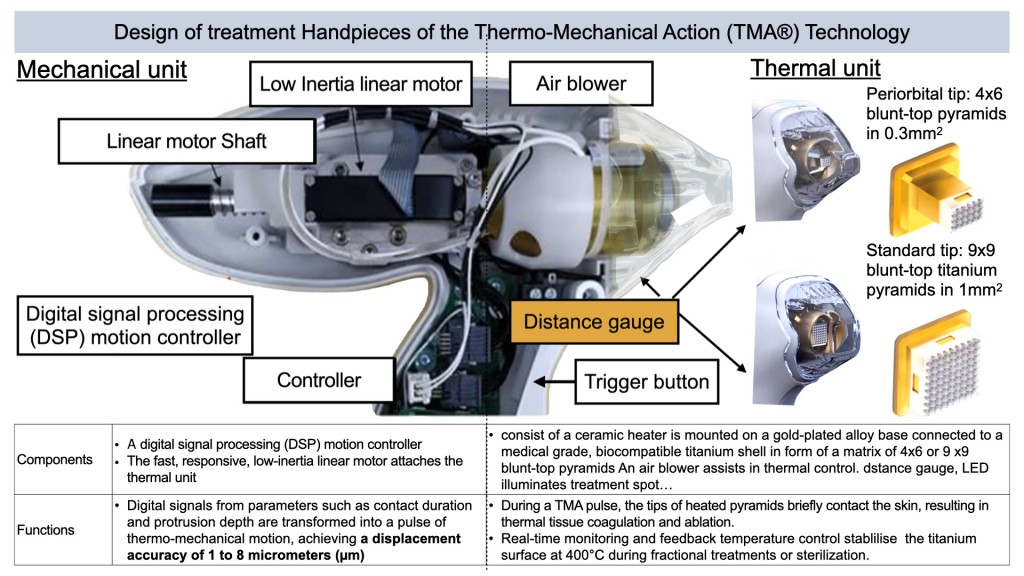
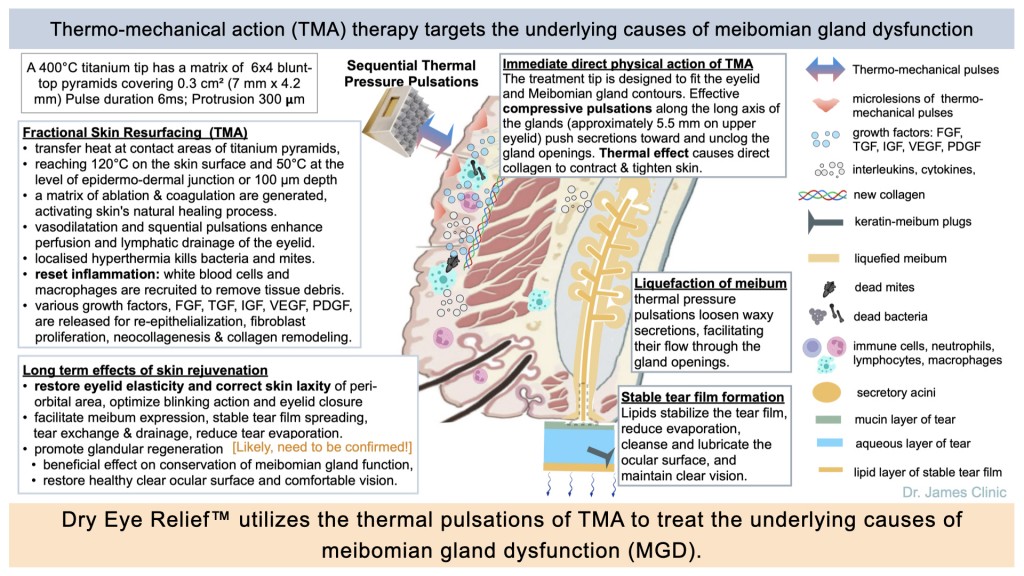
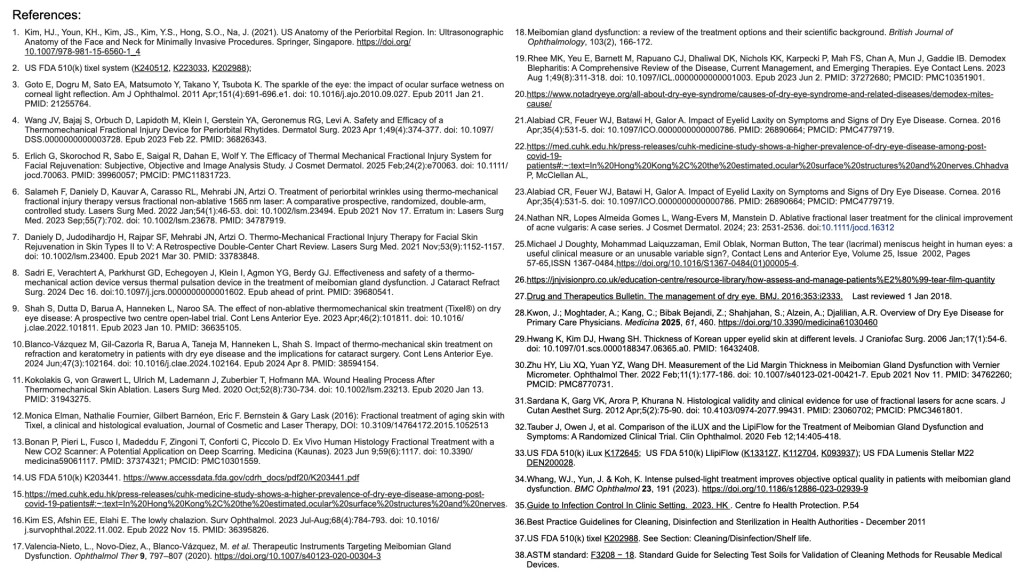
Tixel Sequential Thermal Pulsation Therapy, patented TMA, utilizes thermo-mechanical action to treat dry eye disease (DED), blepharitis, and meibomian gland dysfunction (MGD).
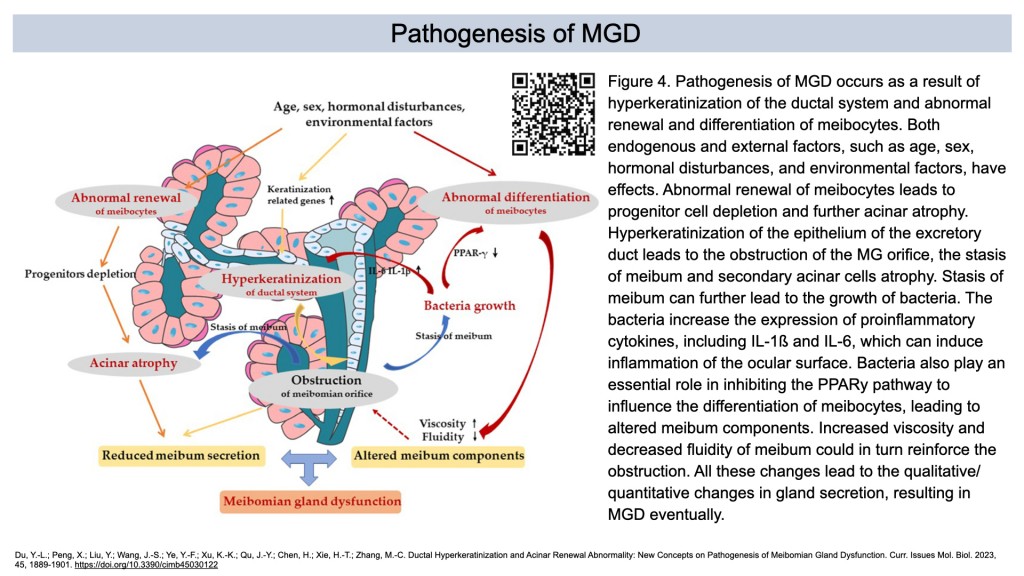
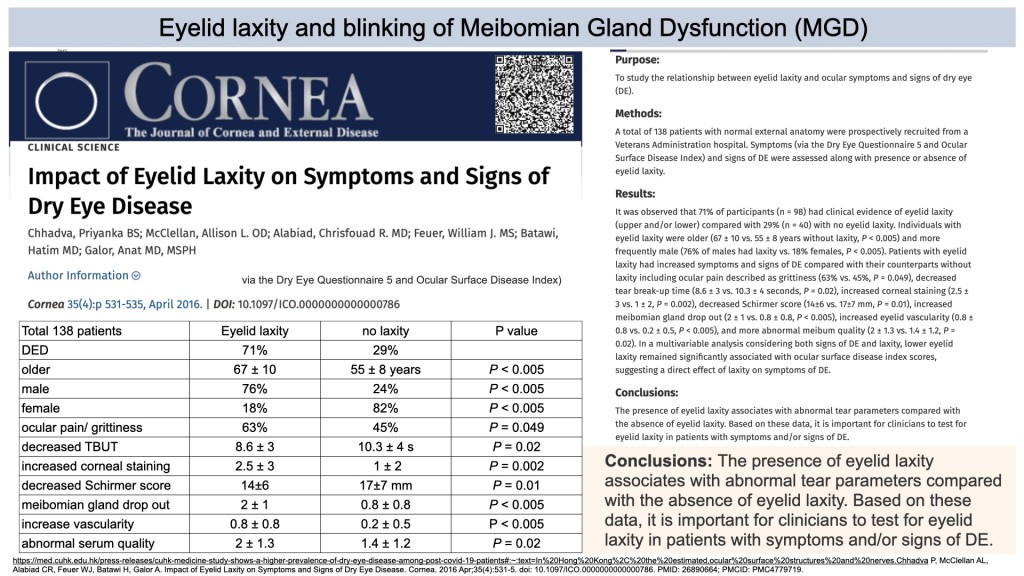
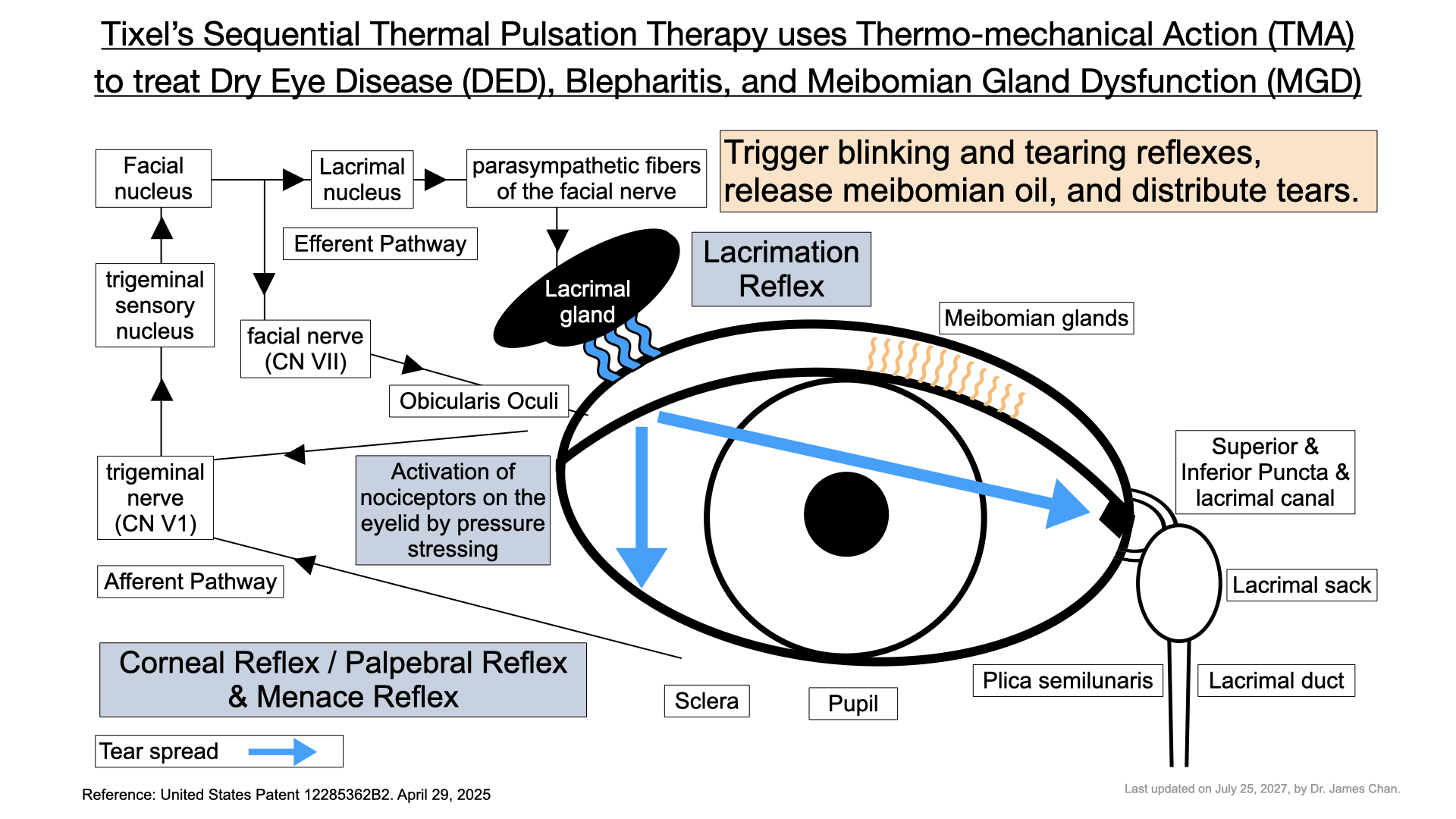
Possible hypotheses of Thermo-mechanical Action targeting the underlying causes of meibomian gland dysfunction
The edited diagrams above are intended for teaching and explanation purposes only and do not represent all final facts. They must be coordinated with continuously updated medical research reports. This serves as a declaration.
以上編輯的圖片是為了教學和解釋的方便,並不代表全部的最終事實。它們仍需與不斷更新的醫學研究報告結果相協調。特此聲明。