Part III. Thermo-mechanical Action Tixel TMA: Mechanisms for controlling the advancement and retraction of mechanical motion and heat transfer.
 |
Dr James |
Part 1. Clinical studies (last updated on 2025-08-30)
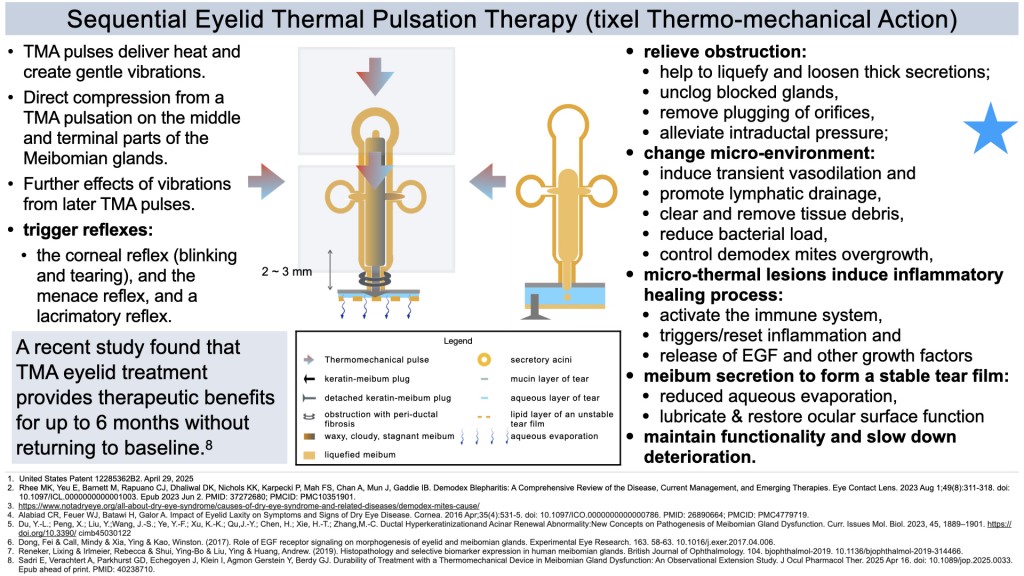
Sequential thermal pulsations of TMA treat the underlying causes of evaporative dry eye caused by meibomian gland dysfunction (MGD).
Part 2. Illustrations of ‘Dermal Conditioning’ with Thermo-Mechnanical Action (last updated on 2025-08-30)
For reference only, please refer to the original article for the information.
大雨過後,蚊蟲滋生特別嚴重。除文中的資料外,我編輯了一些補充資料給大家參考。
以下是來自美國CDC之參考資料 2025年4月23日
有效的外用驅蟲劑
美國環保署 (EPA) 註冊的驅蟲劑已被證明能有效減少蚊子、白蛉等昆蟲以及蜱蟲和蟎蟲等節肢動物的叮咬。 EPA 註冊產品在按照指示使用時被認為是安全的,即使是孕婦和哺乳期婦女也適用。美國疾病管制與預防中心 (CDC) 已評估同行評審的科學文獻中發表的資訊以及 EPA 提供的數據,並確定了幾種能夠安全有效地預防昆蟲叮咬的 EPA 註冊產品。含有以下活性成分的產品通常能夠提供相當持久的防護:
美國環保署 (EPA) 將活性成分 DEET 和派卡瑞丁歸類為「傳統」驅蟲劑。生物農藥驅蟲劑(OLE、PMD、IR3535 和 2-十一酮)則源自天然材料,或為天然材料的合成版本。
Cipeller PMD 是一款以 PMD(對薄荷烷-3,8-二醇)為活性成分的驅蚊產品。 PMD 是一種源自檸檬香味橡膠樹的天然化合物。 Cipeller PMD 產品旨在驅除蚊子、蠓蟲、蜱蟲和蒼蠅,部分配方可提供長達 8 小時的防護。
以下是更細緻的成分:
* 活性成分:Cipeller PMD 產品含有植物性驅蟲劑 PMD。
* 有效性:經證實,PMD 在驅除蚊子和其他昆蟲方面與 DEET 相當。
* 安全性:Cipeller PMD 通常採用不含 DEET 和樟腦的配方,適合兒童和成人使用。
* 應用:Cipeller PMD 產品有多種形式,包括噴霧劑和濕紙巾,可用於皮膚或衣物。
* 認可:美國疾病管制與預防中心 (CDC) 認可 PMD 是一種安全有效的驅蚊劑。
當需要同時使用驅蚊劑及防曬用品時
一般來說,應分開使用,先塗防曬霜,然後再使用驅蟲劑。由於使用含避蚊胺 (DEET) 的驅蟲劑會導致防曬係數 (SPF) 降低,因此可能需要更頻繁地補充防曬霜。防曬霜和驅蟲劑的使用方法均應遵循製造商的說明。
This is a set of clinical photos of Thermomechanical Action (TMA) technology, an effective treatment for evaporative dry eye disease, Demodex blepharitis, and meibomian gland dysfunction (MGD). MGD is the commonest cause of dry eye disease. MGD is a common cause of blepharitis and is often associated with Demodex infestation.
In humans, there are two types of demodex mites on the skin, Demodex folliculorum and Demodex brevis. Demodex folliculorum mites are longer and primarily cluster in human hair follicles, particularly on the face and eyelids, inhabiting the eyelash follicles. They are also found in the sebaceous glands and Meibomian glands. Demodex brevis mites are shorter and exist solitary in the meibomian glands of the eyelids. These mites are believed to contribute to meibomian gland dysfunction (MGD), which can cause dry eye symptoms. Demodex brevis infests the meibomian glands, which produce oil (sebum) that lubricates the eye and helps keep the tear film stable.
Demodex mites are common commensals, meaning they can be present on the skin without causing any symptoms. However, the overgrowth of Demodex mites causes problems like blepharitis, dry eyes due to meibomian gland dysfunction, and rosacea. Demodex blepharitis is especially common in patients over the age of 60.
The following photo is the eyelid of a 65-year-old lady suffering from dry eye disease with compensatory watery tearing. There is evidence of a Demodex mite infestation. These tiny, microscopic parasites live in or near hair follicles, particularly around eyelashes and eyebrows. Cuffing, seen here, is a classic symptom of Demodex overpopulation. The accumulation of degenerated, hyperkeratinized cellular debris with sebum and lipid creates the familiar sign of cuffs, cylindrical dandruff, or “sleeves” commonly seen at the base of the lashes in patients who have D. folliculorum infestation. There is also some debris on the ocular surface, which signifies an unhealthy status of the ocular surface.
The patient had one session of tixel treatment with the Thermo-mechanical Action (TMA) of the eyelid, a USA FDA-cleared indication. Following the treatment, her dry eye symptoms and inflammation from blepharitis progressively improved. Two months after the procedure, the number of Demodex mites on her eyelid significantly decreased. The dry eye symptoms were alleviated. As a result, the patient no longer required eyedrops for her dry eye condition post-treatment.
A recent clinical study * found that the thermomechanical device TMA is safe and effective for improving signs and symptoms of evaporative dry eye disease in MGD, with benefits lasting up to 6 months. No ocular adverse effects were reported.

Post-treatment photo. Tixel Eyelid Thermal Pulsation Therapy with the Thermo-mechanical Action (TMA) dry eye disease Relief. Two months after the procedure, the eyelid is healthy without overgrowth of demodex mites.
這是熱機械作用 (TMA) 技術的一組臨床照片證據,該技術可以有效治療蒸發過強的乾眼症、蠕形蟎性瞼緣炎和瞼板腺功能障礙。瞼板腺功能障礙是乾眼症最常見的原因, 也是瞼緣炎的常見原因,通常與蠕形蟎蟲感染有關。
在人類中,皮膚上有兩種類型的蠕形蟎,毛囊蠕形蟎和短蠕形蟎。毛囊蠕形蟎較長,主要聚集在人類的毛囊中,尤其是臉部和眼瞼,棲息於睫毛毛囊。它們也存在於皮脂腺和瞼板腺中。短蠕形蟎體型較短,單獨存在於眼瞼的瞼板腺。這些蟎蟲被認為會導致瞼板腺功能障礙(MGD),進而引起乾眼症症狀。短蠕形蟎寄生於瞼板腺,瞼板腺會產生油脂(皮脂),潤滑眼睛並幫助維持淚膜穩定。
蠕形蟎是常見的共生體,這意味著它們可以存在於皮膚上但不會引起任何症狀。然而,蠕形蟎的過度生長會引起瞼緣炎、瞼板腺功能障礙引起的眼睛乾澀以及酒渣鼻等問題。蠕形蟎性瞼緣炎在 60 歲以上的患者中尤其常見。
下圖是一位65歲患有乾眼症的女士的眼瞼,並伴隨著代償性流淚。有證據顯示有蠕形蟎感染。這些微小的寄生蟲生活在毛囊內或附近,尤其是睫毛和眉毛周圍。這裡看到的袖口是蠕形蟎過度繁殖的典型症狀。退化的、角質化的細胞碎片與皮脂和脂質一起積聚,形成了我們熟悉的袖口、圓柱形頭皮屑或「袖子」症狀,常見於感染毛囊蠕形蟎的患者的睫毛根部。眼表上還存在一些碎屑,顯示眼表狀態不健康。
該患者接受了一次眼瞼熱機械作用 (TMA) 的 tixel 治療,這是美國 FDA 批准的適應症。經過治療,她的乾眼症症狀和瞼緣炎引起的發炎逐漸改善。手術兩個月後,她眼瞼上的蠕形蟎蟲數量明顯減少。乾眼症狀得到緩解。結果,治療後患者不再需要滴眼藥水來治療乾眼症。
最近的臨床研究發現,TMA 熱機械眼瞼治療可安全有效地改善 MGD 蒸發性乾眼症的徵兆和症狀,且療效可持續長達 6 個月。報告沒有發現眼部不良反應。
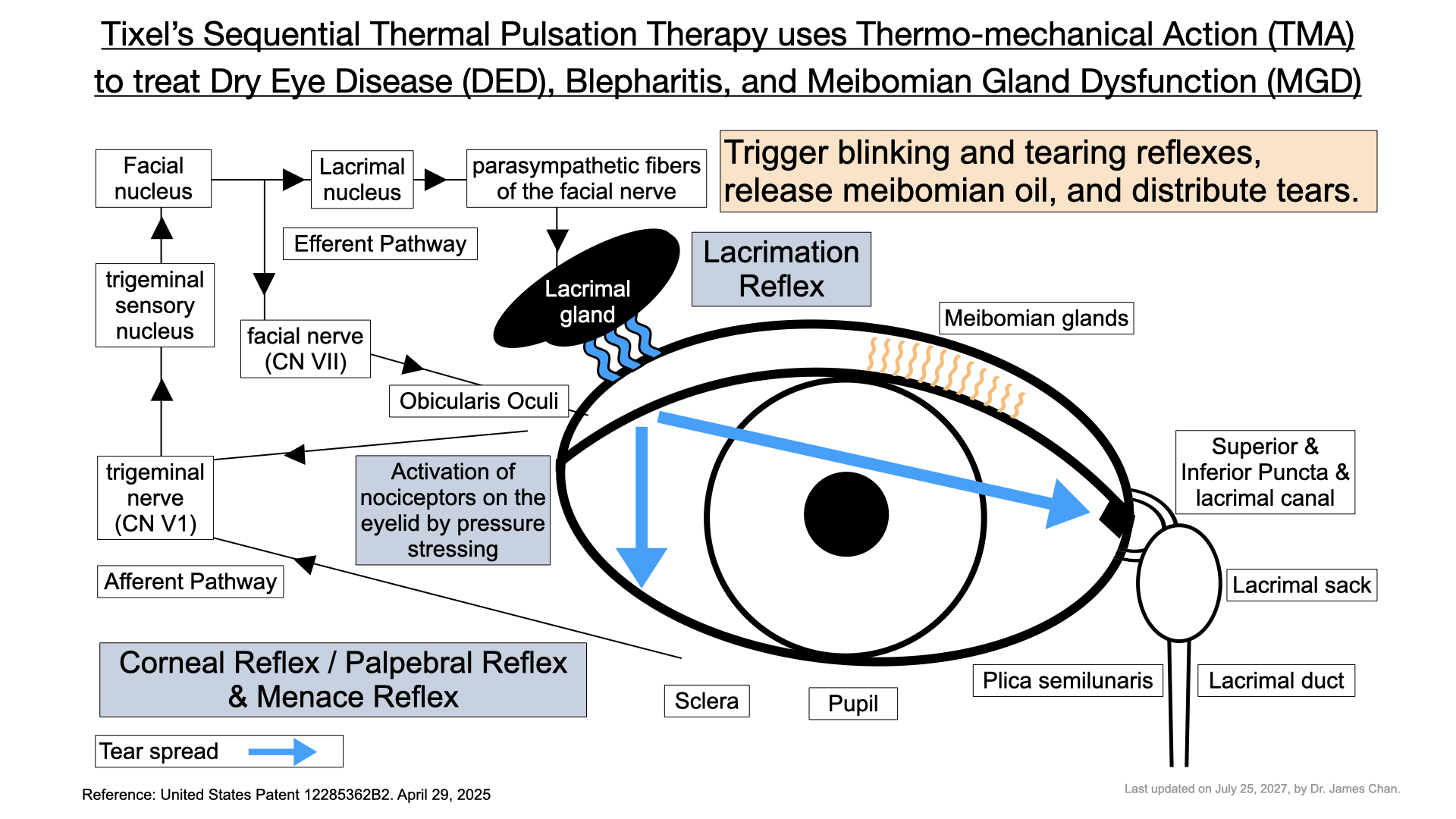
Tixel Sequential Thermal Pulsation Therapy, patented TMA, utilizes thermo-mechanical action to treat dry eye disease (DED), blepharitis, and meibomian gland dysfunction (MGD).
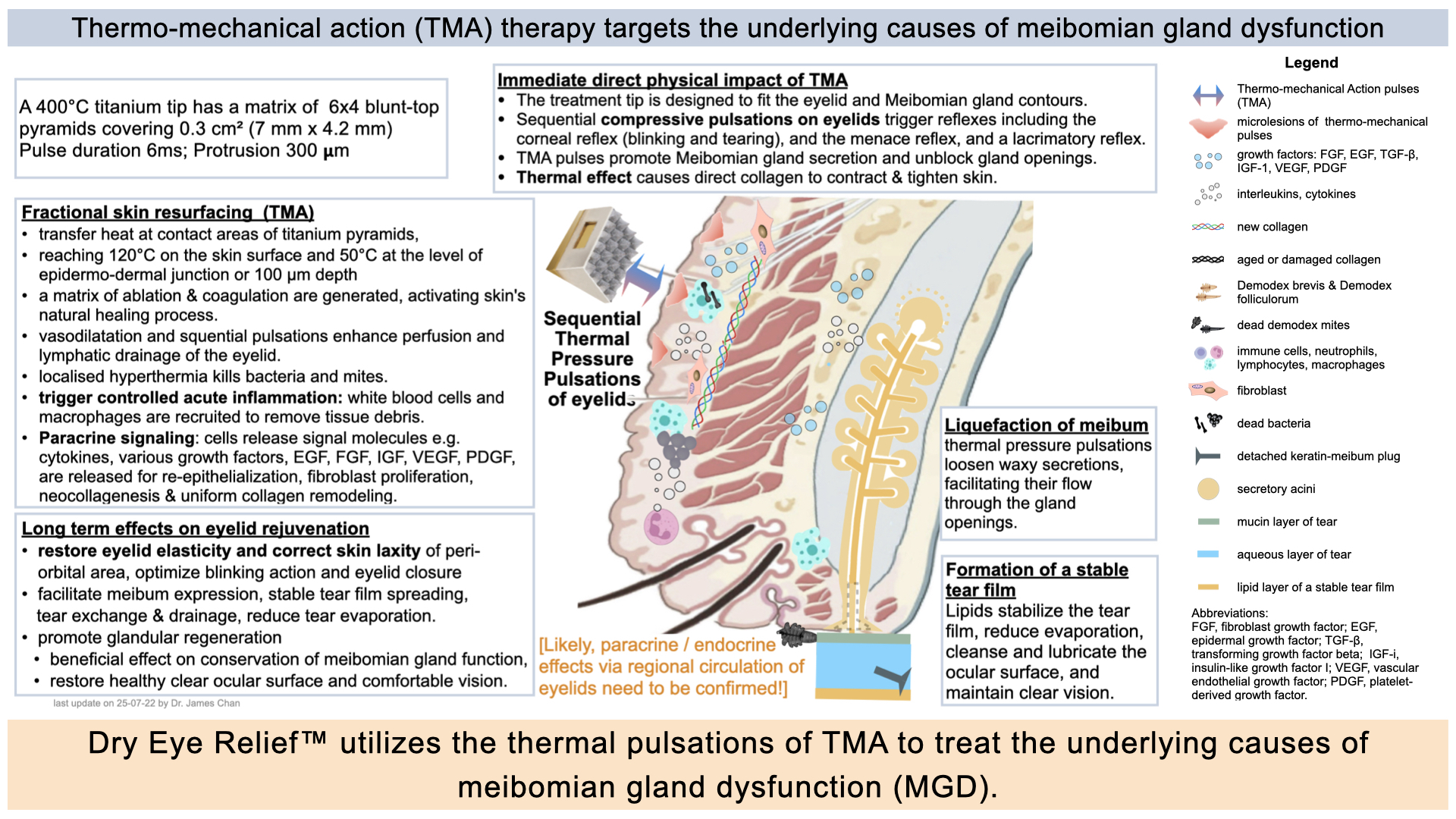
Possible hypotheses of Thermo-mechanical Action targeting the underlying causes of meibomian gland dysfunction
The edited diagrams above are intended for teaching and explanation purposes only and do not represent all final facts. They must be coordinated with continuously updated medical research reports. This serves as a declaration.
以上編輯的圖片是為了教學和解釋的方便,並不代表全部的最終事實。它們仍需與不斷更新的醫學研究報告結果相協調。特此聲明。
與乾眼症 (DED) 和瞼板腺功能障礙 (MGD) 相關的藥物包括口服避孕藥,由於其含有雌激素和黃體素,可能導致與 MGD 相關的乾眼症。用於治療攝護腺(前列腺)問題的坦索羅辛和特拉唑嗪也與乾眼症有關。某些抗癌藥物,如甲胺蝶呤和西妥昔單抗,會影響淚腺,導致乾眼症。此外,常用於治療胃灼熱的質子幫浦抑制劑 (PPI) 也可能透過維生素 B12 缺乏或影響腸道菌叢而導致乾眼症。
局部用藥時,苯扎氯銨 (BAK) 是一種存在於許多眼藥水中的防腐劑,它與乾眼症和 MGD 密切相關,因為它會破壞淚膜。許多青光眼藥物也含有 BAK,長期使用會加重乾眼症。
其他可能導致乾眼症 (DED) 和瞼板腺分泌障礙 (MGD) 的因素包括配戴隱形眼鏡(這會加劇症狀)以及眼瞼衛生不良(會導致細菌積聚,從而對瞼板腺分泌產生負面影響)。蠕形蟎在這些疾病中的作用仍在研究中,但一些研究表明其與瞼板腺分泌障礙 (MGD) 有關,尤其是在乾眼症 (DED) 患者中。
治療方法包括透過熱敷、眼瞼按摩和眼瞼擦洗來保持眼瞼衛生,以改善瞼板腺分泌。脂質類人工淚液有助於穩定淚膜,而局部或全身性用藥則可根據 DED/MGD 的嚴重程度進行。診室內操作,例如瞼板腺擠壓術或 LipiFlow,可以幫助疏通阻塞的腺體。
Medications associated with Dry Eye Disease (DED) and Meibomian Gland Dysfunction (MGD) include oral contraceptives, which can lead to MGD-related dry eye due to their estrogen and progesterone content. Tamsulosin and terazosin, used for prostate issues, are also linked to DED. Certain anticancer drugs, such as methotrexate and cetuximab, can affect the lacrimal glands, contributing to dry eye. Additionally, proton pump inhibitors (PPIs), commonly used for heartburn, may cause DED through vitamin B12 deficiency or impacts on the gut microbiome.
Topically, benzalkonium chloride (BAK), a preservative found in many eye drops, is strongly associated with DED and MGD as it disrupts the tear film. Many glaucoma medications contain BAK as well and can worsen dry eye with prolonged use.
Other factors that can contribute to DED and MGD include contact lens wear, which can exacerbate symptoms, and poor eyelid hygiene that allows bacteria to accumulate, thereby negatively affecting meibomian gland secretion. The role of Demodex mites in these conditions is still under investigation, though some studies suggest a link with MGD, particularly in patients with DED.
Treatment options include maintaining eyelid hygiene through the use of warm compresses, eyelid massage, and lid scrubs to improve meibomian gland flow. Lipid-based artificial tears can help stabilise the tear film, while topical or systemic medications may be prescribed based on the severity of DED/MGD. In-office procedures, such as meibomian gland expression or LipiFlow, can help clear blocked glands.
瞼板腺是人體中最辛勤工作的組織之一。它們晝夜不停地運作,製造足夠的油脂分泌出來,凝成及維持穩定的淚膜,減少淚液蒸發,潤滑和保護眼球表面,並確保清晰的視力。這些腺體位於眼瞼內,隨著年齡的增長,以及環境因素和其他影響的影響,它們的數量會逐漸減少。並失去油脂分泌功能,最終萎縮。
瞼板腺功能障礙的初期症狀通常很輕微,許多人可能只是偶爾使用潤滑眼藥水。因此,他們可能直到感到不適才意識到問題所在,而不適通常是在腺體功能嚴重喪失後出現的。當您開始感到嚴重的眼睛不適時,您的瞼板腺功能可能已經喪失了近一半。
雖然一般的居家照護措施(例如使用熱敷、保持眼瞼衛生、保持眼部衛生以及服用歐米伽-3等營養補充劑)可能有所幫助,但它們只是輔助性質。有效的治療需要在診所進行專業的治療。如果沒有及時適當的護理,可能會出現更嚴重的症狀,導致眼球表面損傷、視力模糊,並嚴重影響生活品質。
近年在乾眼症及治療瞼板腺功能障礙的技術上,也突破性的發展。現在更了解清楚乾眼症的成因及病理,可以針對性,精準地,同時處理多方面的病因。更有效,快速及安全地治療,在短時間內改善乾眼徵狀、且效果更可維持半年或以上。
Meibomian glands are among the hardest-working tissues in the body. They work around the clock to produce enough oily secretion to form and maintain a stable tear film, reduce tear evaporation, lubricate and protect the surface of the eyeball, and ensure clear vision. These glands are located in the eyelids, and as we age, along with exposure to environmental factors and other influences, their number gradually decreases. They also tend to lose their oil-secreting function and can eventually atrophy.
The initial symptoms of meibomian gland dysfunction are often subtle, and many people may only occasionally use lubricating eye drops. As a result, they may not recognise the problem until they experience discomfort, which can occur after a significant loss of gland function. By the time you start experiencing substantial eye discomfort, you may have already lost nearly half of your meibomian gland function.
While general home care practices—such as using warm compresses,
Lipid-based artificial tears, maintaining lid hygiene, practicing eye hygiene, and taking nutritional supplements like omega-3—can be helpful, they are only supplementary. Effective treatment requires professional intervention at an ophthalmology clinic. Without timely and appropriate care, more serious symptoms can develop, leading to damage to the eyeball’s surface, blurred vision, and a significant impact on one’s quality of life.
In recent years, there have been breakthroughs in the technology of dry eye and treatment of meibomian gland dysfunction. Now we have a better understanding of the causes and pathology of dry eye, and we can treat multiple causes in a targeted, precise and simultaneous manner. More effective, fast and safe treatment can improve dry eye symptoms in a short period of time, and the effect can last for half a year or more.
乾眼症 (DED) 是一種高度流行的眼部疾病,其特徵是淚膜和眼表穩態的改變。根據香港中文大學 2022 年的一項調查,約有 30% 的人口患有乾眼症。值得注意的是,80% 的乾眼症病例是脂質缺乏性或蒸發過強型乾眼症,是由瞼板腺功能障礙 (MGD) 引起的。因此,瞼板腺功能障礙影響著數百萬人,尤其是在亞洲國家。
瞼板腺功能障礙 (MGD) 患者的眼瞼油脂分泌腺無法分泌足夠或適當的油脂,從而導致乾眼症狀。這些位於眼瞼邊緣的腺體負責分泌瞼脂,這種油性物質可以保護淚膜,防止淚膜過快蒸發,並保持眼部濕潤健康。
瞼板腺功能障礙 (MGD) 可發生在所有年齡層的人群中,尤其是 60 歲以上的人。導致 MGD 的因素有很多,包括老化、荷爾蒙變化、低濕度以及低 Omega-3 脂肪酸或高 Omega-6 脂肪酸的飲食。
其他促成因素包括配戴隱形眼鏡以及某些局部或全身用藥。長時間使用電子設備會導致眨眼頻率降低和眼瞼閉合不全,進而導致淚膜蒸發增加、不穩定,以及淚液滲透壓升高。長時間使用螢幕也可能是兒童和青少年乾眼症 (DED) 發病率上升的一個因素。
在瞼板腺功能障礙 (MGD) 病例中,由眼瞼中的瞼板腺分泌的油性分泌物(稱為瞼脂)分泌份量不足且成分改變。這會導致分泌物增厚、混濁且停滯,更難以擠出。如果沒有足夠的油脂分泌,由黏蛋白、水和油脂組成的健康淚膜層就無法正常形成。
促成因素包括淚膜不穩定、水份蒸發率增加、乾燥、淚液高滲透壓、發炎。眼球表面潤滑不足,導致眼瞼和眼球之間產生摩擦,令眼表細胞受損。這些問題會導致淚液代償性分泌過剩,從而形成乾眼症 (DED) 的持續循環。
乾眼症 (DED) 的眼睛症狀包括乾澀、眼部異物感、眼部疲勞、眼紅、灼熱或疼痛、視力模糊、畏光以及作為代償反應的過度流淚。 DED 也與眼瞼發炎和感染(例如瞼緣炎)以及蠕形蟎蟲感染有關。
總結: 瞼板腺功能障礙 (MGD) 是一種慢性進行性疾病,會危害眼表健康。如果不及時治療,MGD 可能會惡化,導致嚴重症狀、持續不適、角膜損傷、眼部感染以及潛在的嚴重視力障礙。優先考慮有效的醫學治療對於確保您的眼部健康和維持生活品質至關重要。
Dry eye disease (DED) is a highly prevalent ocular condition that is characterised by alterations in the homeostasis of the tear film and the ocular surface. According to a 2022 survey conducted by the Chinese University of Hong Kong, approximately 30% of the population suffers from DED. Notably, 80% of DED cases are lipid-deficient or evaporative dry eye, which is caused by Meibomian gland dysfunction (MGD). As a result, meibomian gland dysfunction affects millions of people, especially in Asian countries.
In patients with Meibomian gland dysfunction (MGD), the oil-secreting glands in the eyelids fail to produce enough oil or produce the wrong type of oil, resulting in dry eye symptoms. These glands, located at the edges of the eyelids, are responsible for creating meibum, an oily substance that protects the tear film. This helps prevent the tear film from evaporating too quickly, keeping the eyes moist and healthy.
Meibomian Gland Dysfunction (MGD) can occur in individuals of all age groups, especially in those over 60. Several factors contribute to MGD, including aging, hormonal changes, low humidity, and diets that are low in omega-3 fatty acids or high in omega-6 fatty acids.
Other contributing factors include the use of contact lenses and certain topical or systemic medications. Extended use of electronic devices can lead to decreased blink rates and incomplete eyelid closure, which results in increased evaporation and instability of the tear film, as well as higher tear osmolarity. Prolonged screen time may also be a factor in the rising rates of dry eye disease (DED) among children and young adults.
In cases of Meibomian Gland Dysfunction (MGD), the oily secretion known as meibum, which is produced by the meibomian glands in the eyelids, is often insufficient in quantity and altered in composition. This leads to a thickened, cloudy, and stagnant secretion that is more difficult to express. Without adequate oil, the healthy layers of the tear film—comprising mucin, water, and oil—cannot form properly.
Contributing factors include tear film instability, increased evaporation rate, dryness, tear hyperosmolarity, and inflammation. Inadequate lubrication of the eye surface causes friction between the eyelid and eyeball, which damages the cells on the eye surface. These problems lead to compensatory overproduction of tears, which creates a perpetuating cycle of dry eye disease (DED).
Ocular symptoms of Dry Eye Disease (DED) can include dryness, a gritty sensation, eye fatigue, redness, burning or pain, blurred vision, sensitivity to light, and excessive tearing as a compensatory response. DED is also associated with eyelid inflammation and infections, such as blepharitis, as well as infestations by Demodex mites.
Summary: Meibomian gland dysfunction (MGD) is a chronic, progressive disease that compromises the health of the ocular surface. If left untreated, MGD can worsen, leading to severe symptoms, ongoing discomfort, corneal damage, eye infection, and potentially serious visual impairment. Prioritizing effective medical treatment is critical to ensuring your eye health and maintaining quality of life.
From Basic to Advance - The Art and Science of Periorbital Rejuvenation
Association of Doctos in Aesthetic Medicine (Hong Kong) (ADAM) in colloboration with Hong Kong Society of Ophthalmic Plastic and Reconstructive Surgery (HKSOPRS)
‘Transformative Periorbital Skin Rejuvenation & Dry Eye ReliefTM by Patented Thermo-mechanical Action’ presented by Dr. James Chan
30th March 2025 (Sunday)
Ballroom, Hyatt Regency Hotel
Tsim Sha Tsui
Hong Kong
接種新冠疫苗是保護自己和大家的唯一辦法。
只接種了一針或两針疫苗後,不論是那種疫苗,你仍然無法抵抗Omicron新冠肺炎變種病毒。染病而病徵輕微的你,更不自覺地把病毒散播。
所以必需接種第三針疫苗,最好是復必泰 mRNA疫苗。
衞生防護中心轄下科學委員會建議: 已接種兩劑克爾來福或復必泰疫苗的成年人於接種第二劑三個月後盡快接種第三劑復必泰疫苗。
祝大家身體健康,很快回歸正常生活。
Moderna reported that during the phase 3 study of its vaccine candidate mRNA-1273, which enrolled 30,000 adult U.S. participants, just five of the 95 COVID-19 cases occurred among the vaccinated, while 90 infections were identified in the placebo group. This corresponds to an efficacy of 94.5%. None of the infected patients who received the vaccine developed severe COVID-19, while 11 (12%) of those who received the placebo did.
Similarly, the Pfizer-BioNTech vaccine candidate, BNT162b2, was 90% effective in preventing infection during the phase 3 clinical trial, which enrolled 43,538 participants, with 30% in U.S. and 42% abroad.